Semaglutide & GLP‑1 Weight‑Loss Drugs (Ozempic, Wegovy, Mounjaro): Evidence, Risks, and Real‑World Impact
An evidence-based review of semaglutide and other GLP‑1 agonists as weight‑loss medications, their clinical performance, side effects, access challenges, and how they are reshaping obesity care and public discourse.
Executive Summary
Semaglutide and related GLP‑1 receptor agonists—marketed as Ozempic (semaglutide for type 2 diabetes), Wegovy (semaglutide for obesity), and Mounjaro (tirzepatide; GLP‑1/GIP agonist)—deliver substantially greater average weight loss than older medications and lifestyle modification alone. Large randomized controlled trials show mean body‑weight reductions of roughly 10–20% over 1–2 years in many patients with obesity, alongside improvements in glycemic control and some cardiometabolic risk markers.
These benefits come with trade‑offs: common gastrointestinal side effects, the need for long‑term or indefinite treatment to maintain weight loss, high list prices, and access inequalities driven by insurance coverage and drug shortages. Social media has amplified both success stories and fears, often blurring the line between rigorous evidence and anecdote.
- Best for: Adults with obesity (BMI ≥30) or BMI ≥27 with weight‑related comorbidities, especially type 2 diabetes, when lifestyle changes alone have been insufficient.
- Not ideal for: People seeking rapid “cosmetic” weight loss without medical need; individuals with specific contraindications (e.g., personal/family history of medullary thyroid carcinoma or MEN2 for semaglutide).
- Key decision factors: Cardiometabolic risk, tolerability of GI side effects, ability to afford and access ongoing therapy, and willingness to pair medication with durable lifestyle changes.
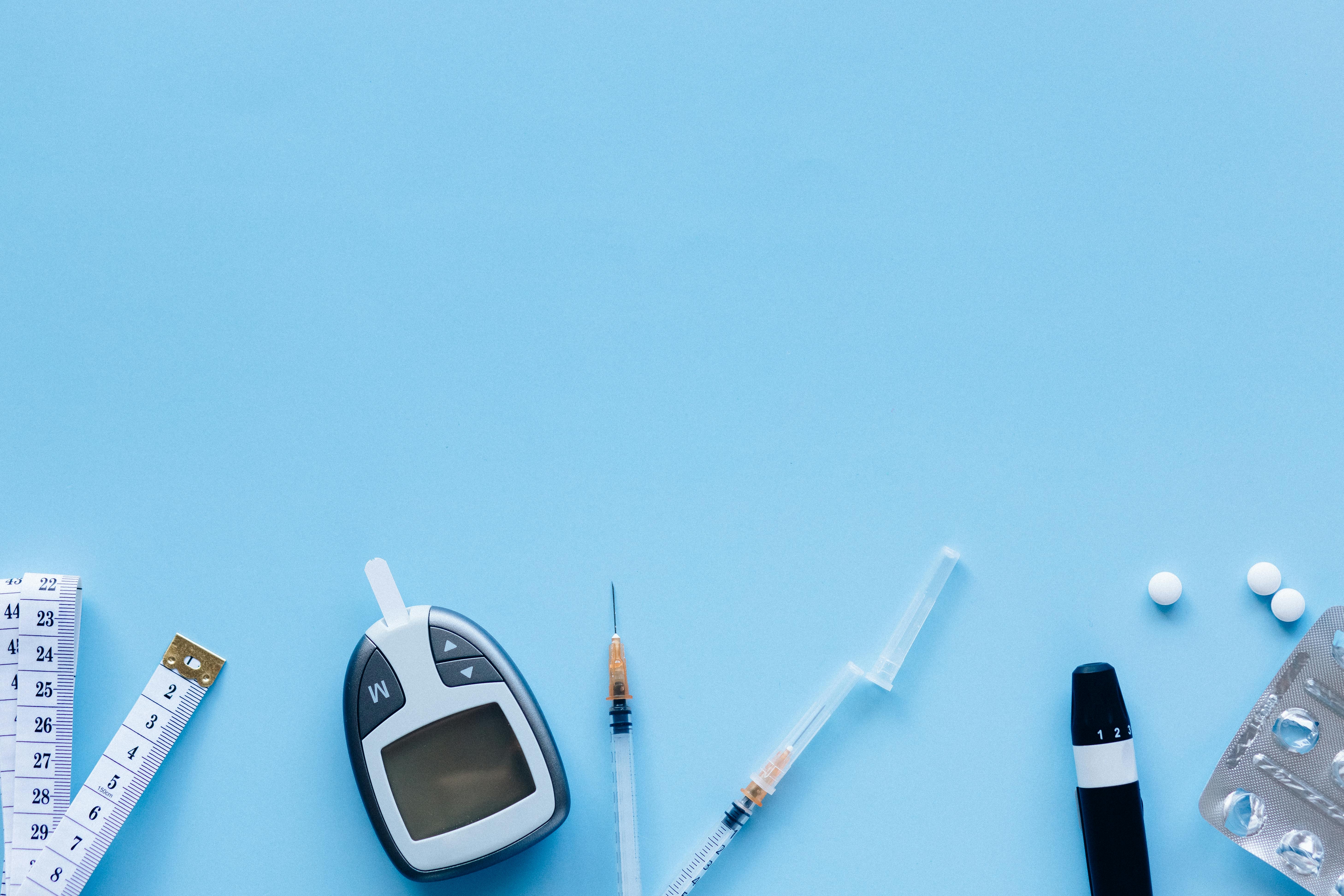
Visual Overview of GLP‑1 Weight‑Loss Treatments
The following images illustrate how GLP‑1 weight‑loss drugs are administered, the physiological pathways they target, and how their real‑world uptake is changing obesity treatment.






Key Drug Specifications and Indications
GLP‑1 receptor agonists (and the related dual agonist tirzepatide) differ in approved indications, dosing, and regulatory status, despite overlapping mechanisms.
| Brand (Generic) | Primary Indication (2026) | Drug Class | Typical Dosing | Approx. Mean Weight Loss* |
|---|---|---|---|---|
| Ozempic (semaglutide) | Type 2 diabetes; cardiovascular risk reduction in high‑risk adults; used off‑label for obesity. | GLP‑1 receptor agonist | Weekly injection; titrated up to 1.0–2.0 mg depending on jurisdiction and indication. | ~5–10% body weight in diabetes trials. |
| Wegovy (semaglutide) | Chronic weight management in adults (and in some regions, adolescents) with obesity or overweight plus comorbidities. | GLP‑1 receptor agonist | Weekly injection; up‑titrated to 2.4 mg semaglutide. | ~15% average weight loss at 68 weeks in major trials. |
| Mounjaro (tirzepatide) | Type 2 diabetes; in some regions also approved for chronic weight management. | Dual GLP‑1/GIP receptor agonist | Weekly injection; maintenance doses often 5–15 mg. | Up to ~20% average weight loss in obesity trials at higher doses. |
*Approximate ranges from phase 3 trials; individual results vary substantially. For formal prescribing information, see the manufacturer or regulatory authority websites (e.g., Wegovy prescribing information, Ozempic prescribing information, Mounjaro prescribing information).
Mechanism of Action: How GLP‑1 Drugs Drive Weight Loss
GLP‑1 (glucagon‑like peptide‑1) is an incretin hormone released by the gut in response to food intake. GLP‑1 receptor agonists are synthetic molecules that mimic or enhance this signal, with longer duration of action than the body’s native hormone.
- Appetite modulation in the brain: GLP‑1 receptors in the hypothalamus and other brain regions help regulate satiety. Agonists reduce hunger and cravings, particularly for high‑calorie foods, leading to
effort feels lower
when patients attempt caloric restriction. - Slowed gastric emptying: Food leaves the stomach more slowly, enhancing fullness after smaller meals. This effect is strongest early in treatment and contributes both to weight loss and to common GI side effects like nausea.
- Improved glycemic control: In people with type 2 diabetes, GLP‑1 agonists enhance glucose‑dependent insulin secretion and suppress glucagon, reducing fasting and postprandial blood glucose and contributing to lower A1C values.
- Secondary cardiometabolic effects: Some GLP‑1 drugs have demonstrated reduced major cardiovascular events in high‑risk patients, though the mechanisms likely extend beyond weight loss alone (e.g., effects on inflammation, blood pressure, and lipids).
The net effect is reduced energy intake without the same degree of compensatory hunger that typically undermines diet‑only approaches. However, energy expenditure can also fall as body weight declines, which is why lifestyle strategies still matter to maintain long‑term balance.
Clinical Efficacy vs. Real‑World Outcomes
Pivotal trials such as STEP (semaglutide) and SURMOUNT/SURPASS (tirzepatide) have transformed clinical expectations for non‑surgical weight management.
- Average weight loss: Wegovy (semaglutide 2.4 mg) has demonstrated ~15% mean weight loss at ~68 weeks in people with obesity; tirzepatide in some trials has approached or exceeded 20% at higher doses.
- Clinically meaningful thresholds: Many patients achieve ≥5–10% weight loss, a range associated with improvements in blood pressure, lipids, glycemic control, and sleep apnea severity.
- Cardiovascular outcomes: GLP‑1 therapies have shown reductions in composite cardiovascular endpoints in high‑risk individuals with type 2 diabetes. Ongoing studies are clarifying benefits specifically in obesity without diabetes.
Real‑world effectiveness is more variable. Adherence drops over time due to side effects, cost, or access issues, and some patients lose less weight than trial averages. In practice, clinicians typically reassess after 3–6 months: if weight and metabolic parameters are not improving adequately, they may adjust the dose, address lifestyle barriers, or consider alternative approaches.
Social Media, Public Perception, and the “Ozempic Trend”
GLP‑1 drugs have moved from specialist clinics into mainstream conversation. On platforms like TikTok, Instagram, and YouTube, users document week‑by‑week progress, side‑effect management, and clothing size changes under hashtags referencing Ozempic, Wegovy, and Mounjaro.
This user‑generated content has several implications:
- Normalization of medical treatment for obesity: Many creators describe obesity as a chronic disease, not a failure of willpower, aligning with evolving medical consensus.
- Expectation inflation: Before‑and‑after images often highlight outlier results, which can create unrealistic expectations about speed and magnitude of weight loss.
- Peer support and crowdsourced tips: Users share strategies for coping with nausea, adjusting meal timing, or communicating with clinicians, which can be helpful but is not a substitute for medical advice.
- Misinformation risk: Unverified dosing advice, off‑label combinations, and encouragement to obtain drugs from non‑regulated sources pose safety concerns.
GLP‑1 medications should be viewed as tools within a comprehensive obesity‑care strategy, not as social media challenges or cosmetic shortcuts.
Safety Profile, Side Effects, and Long‑Term Uncertainties
GLP‑1 agonists have been used for diabetes for more than a decade, and their safety profile is relatively well characterized. However, the higher obesity‑treatment doses and long‑term, large‑scale use for weight management raise new questions under active investigation.
Common Side Effects
- Gastrointestinal: Nausea, vomiting, diarrhea, constipation, abdominal pain, and bloating are the most frequent complaints, especially during dose escalation.
- Reduced appetite and taste changes: Often desired for weight loss, but in some cases lead to inadequate nutrient intake if not monitored.
- Injection‑site reactions: Mild redness, swelling, or itching at the injection site.
- Fatigue or malaise: Some users report transient low energy, particularly early in treatment.
Serious Risks and Warnings
- Pancreatitis: A rare but serious risk; patients should seek urgent care for severe, persistent abdominal pain.
- Gallbladder disease: Rapid weight loss increases the risk of gallstones; GLP‑1 use has been associated with cholelithiasis and cholecystitis in some studies.
- Thyroid C‑cell tumors in rodents: Semaglutide and similar agents carry boxed warnings about medullary thyroid carcinoma in animal models. They are contraindicated in individuals with personal/family history of MTC or MEN2, though human relevance is still being studied.
- Hypoglycemia with concomitant therapy: Particularly when combined with insulin or sulfonylureas in diabetes treatment.
Long‑Term and Off‑Treatment Questions
Key open issues include:
- Durability of weight loss after discontinuation: Studies show substantial weight regain when treatment stops, emphasizing the chronic‑disease model of obesity care.
- Impact of decades‑long exposure: As more patients start therapy at younger ages, long‑horizon data will be critical to fully understand cumulative risks and benefits.
- Psychological impact: Some individuals report anxiety about dependence on medication or body‑image concerns related to rapid change. Ongoing psychosocial support is advisable.
Access, Cost, and Policy Debates
Rapid uptake of GLP‑1 drugs has stressed supply chains and highlighted disparities in healthcare access. In some regions, intermittent shortages have forced prioritization of diabetes patients over those seeking treatment for obesity alone.
Pricing and Insurance Coverage
List prices for agents like Wegovy and Mounjaro remain high, often exceeding hundreds of dollars per month. Actual costs depend on:
- National health system policies or formularies.
- Private insurance coverage criteria and prior‑authorization rules.
- Patient‑assistance or manufacturer discount programs.
Many insurers restrict coverage to patients meeting strict BMI and comorbidity thresholds, or require documented prior attempts at lifestyle modification. As long‑term outcome data accumulate, payers are reassessing how to balance upfront drug costs against potential savings from reduced complications of obesity and diabetes.
Ethical and Equity Considerations
- Medical need vs. cosmetic framing: Framing GLP‑1 drugs as “celebrity slim shots” risks minimizing their legitimate role in treating a serious chronic disease.
- Impact of shortages on diabetes care: Off‑label and cosmetic use have, at times, limited availability for patients who rely on these drugs for glycemic control.
- Global inequities: High costs, regulatory delays, and limited infrastructure mean many low‑ and middle‑income countries have minimal access, despite high obesity burdens.
Comparison With Other Weight‑Management Options
GLP‑1 drugs occupy a middle ground between lifestyle‑only approaches and bariatric surgery in terms of average weight loss and invasiveness.
| Approach | Typical Weight Loss | Pros | Cons |
|---|---|---|---|
| Lifestyle interventions alone | ~3–8% with structured programs | Non‑pharmacologic, broadly accessible, multiple health benefits beyond weight. | Hard to sustain at scale; substantial weight regain common. |
| Older oral medications | ~3–9% | Oral dosing; lower cost for some agents. | Less potent on average; some have unfavorable side‑effect or safety profiles. |
| GLP‑1 / dual agonists (Wegovy, Mounjaro) | ~10–20% | High efficacy; cardiometabolic benefits; non‑surgical. | Injectable; GI side effects; high cost; need for ongoing therapy. |
| Bariatric surgery | ~25–35% or more | Most durable weight loss; strong evidence for remission of diabetes and improved survival. | Invasive; surgical risks; requires life‑long nutritional monitoring. |
Real‑World Use and Evidence Evaluation
Unlike consumer products, medications are principally evaluated through clinical trials and post‑marketing surveillance, not informal product testing. For this review, the focus is on:
- Regulatory trial data: Phase 2 and 3 randomized controlled trials forming the basis for approvals in diabetes and obesity.
- Real‑world observational studies: Registry data and insurance‑claims analyses describing adherence, discontinuation, and effectiveness in routine care.
- Pharmacovigilance reports: Adverse‑event databases and safety communications from regulators and manufacturers.
- Clinical practice guidelines: Recommendations from professional societies such as the American Diabetes Association and obesity‑medicine organizations, updated through 2025/2026.
Social‑media testimonials provide anecdotal insight into lived experience but cannot substitute for controlled evidence. Their main value is highlighting patterns—such as challenges with dose escalation or access—that can then be investigated systematically.
Value Proposition and Ideal Candidate Profiles
From a health‑economics perspective, GLP‑1 and dual‑agonist therapies may be cost‑effective in individuals at high risk of obesity‑related complications, particularly when they prevent or delay diabetes, cardiovascular events, or the need for more intensive interventions.
Patients Who May Benefit Most
- Adults with BMI ≥30, or ≥27 with comorbidities such as type 2 diabetes, hypertension, dyslipidemia, or obstructive sleep apnea.
- People with prior unsuccessful attempts at intensive lifestyle change, despite good adherence.
- Patients for whom bariatric surgery is contraindicated, inaccessible, or not preferred.
- Individuals with type 2 diabetes who also need improved glycemic control and cardiovascular‑risk reduction.
Scenarios Where Caution or Alternatives Are Warranted
- Borderline or normal‑weight individuals seeking cosmetic weight loss.
- Patients with contraindications noted in prescribing information (e.g., certain thyroid conditions for semaglutide; history of pancreatitis may require extra caution).
- Individuals unable to commit to regular follow‑up or monitoring of metabolic, nutritional, and psychological status.
- Situations where cost would compromise other essential aspects of healthcare or basic living needs.
Practical User Experience: What Treatment Typically Involves
For patients who start GLP‑1 or dual‑agonist therapy, the day‑to‑day experience is shaped by dosing logistics, side‑effect management, and integration with lifestyle measures.
- Initiation and titration: Therapy usually starts at a low weekly dose and increases every 4 weeks or so, aiming to minimize GI symptoms.
- Routine monitoring: Follow‑up visits or telehealth check‑ins track body weight, glycemic control (where relevant), blood pressure, side effects, and psychological well‑being.
- Dietary adaptations: Smaller, more frequent meals, slower eating, and attention to hydration often help reduce nausea and optimize tolerability.
- Physical activity: Resistance and aerobic training are encouraged both for cardiometabolic benefit and to preserve lean mass during weight loss.
- Planning for the long term: Clinicians and patients should discuss in advance whether treatment is likely to be indefinite and what strategy to follow if medication must be paused or discontinued.
Verdict: How Should Semaglutide and GLP‑1 Weight‑Loss Drugs Be Used?
Semaglutide‑based treatments (Ozempic, Wegovy) and tirzepatide (Mounjaro) represent a substantial advance in the medical management of obesity and type 2 diabetes. They offer levels of weight loss previously seen mainly with bariatric surgery, along with meaningful improvements in glycemic and cardiovascular risk markers for many patients.
At the same time, they are not universal solutions. High cost, supply constraints, side effects, and the need for ongoing use make them best suited for individuals with clear medical indications and access to careful clinical supervision. Public discourse that treats them as quick‑fix aesthetic tools understates both their potential benefits and their risks.
- For clinicians: Integrate GLP‑1 therapies into a comprehensive, long‑term obesity‑care framework, combining pharmacotherapy with nutrition, physical activity, and behavioral support.
- For policymakers and payers: Consider the long‑term health and economic benefits of effective obesity treatment when designing coverage policies, while ensuring equitable access and protecting supplies for diabetes patients.
- For patients: View these medications as powerful tools that can lower the biological barriers to weight loss, but still require engagement with sustainable lifestyle changes and regular medical follow‑up.
Used judiciously and equitably, semaglutide and other GLP‑1 agents can help shift obesity care from blame and short‑term dieting toward chronic‑disease management grounded in biology, evidence, and long‑term support.